Abstract
Day 5 Peripheral Blood Blasts and Day 14 Bone Marrow Studies as Predictors for Response to Therapy in Acute Myeloid Leukemia (AML): An Experience from Indian Subcontinent
Authors
Shilpa Prabhu1, Swasti Sinha1, Vellaichamy M. Annapandian2, Sharat Damodar1, Shoba Badiger1, Sunil Bhat1, K.S. Nataraj1
Author affiliations
1 Department of Hematology and Bone Marrow Transplant, Narayana Health City, Bangalore, India.
2 Department of Academic Research, Narayana Hrudayalaya Foundations, Bangalore, India.
Abstract
Background
The major limitations of treating Acute Myeloid Leukemia (AML) in India are limited resources, patient affordability and utilization of health care services. It is vital to identify easily evaluable prognostic markers to plan for appropriate treatment that enables healthcare providers to deliver treatment at an affordable cost. AML is a most common leukemia in adults and has poor survival and response to treatment. However, with advances in treatment strategies, overall survival has improved in adults and there has been marginal increase in overall survival in older individuals. Studies have showed that immunophenotying to detect blasts by multiparameter flow cytometry on day 5 of induction chemotherapy as a predictor to remission. Financial constraint is the major concern in developing countries, hence peripheral smear examination can be used as an cheaper alternative to look for morphological evidence of blast. Morphological assessment at day 5 peripheral blood blasts can be used as a predictor for remission status, in addition to day 14 bone marrow studies. This strategy will enable us to identify a subset of patients who will benefit from early haematopoeitic stem cell transplant (HSCT) and prognosticate the patients. In this present study we assessed peripheral blast at day5 and day 14 bone marrow studies to predict remission on day 28.
Methods
We analyzed a cohort of 80 AML patients who presented to our centre (Mazumdar Shaw Medical Center, Narayana Health City, Bangalore, India) between April 2013 and April 2017. Diagnosis was confirmed by bone marrow studies based on the morphology, cytochemistry, immunophenotyping and cytogenetics. Clinico-pathological features, immunophenotyping, cytogenetics, mutation profile were recorded at the time of presentation. Day 5 peripheral blood blast percentage, day 14 bone marrow studies (aspiration & biopsy) and day 28 remission bone marrow (or bone marrow done at later dates) studies were recorded.
Results
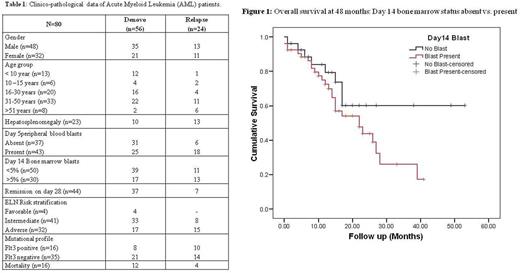
Among 80 patients, 48(60%) were male. The median age was 35 years (range; 10, 59 years). Seventeen (20%) were pediatric patients. Fifty-six (70%) patients were denovo and 24 (30%) were relapse at presentation. The most common presenting symptom was fever 68.75%(n=55). The median WBC count at presentation was 11.95x103/µl (1.5-280 x103). The median blast percentage on the day of diagnosis, day 5 peripheral blood , day 14 bone marrow were 68%, 3% and 4% respectively. According to ELN risk stratification, patients were grouped as favorable risk (3.75%, n=3), intermediate risk (51.25%, n=41) and adverse risk (37.5%, n=30). Thirty eight (47.5%) patients had no blasts in peripheral blood on 5th day of chemotherapy. Of, whom 34(89.4%) had attained remission on day 28 (p<0.01). Day 14 bone marrow blast was absent in 27 cases out of whom 26(96.3%) attained remission on day 28 (p<0.01). The clinicopathological details of the study patients are summarized in table 1.
The overall survival rate was 62% in patients with absence of day 14 bone marrow blast and 32% in patients with persistent disease at the end of 48 months (Figure 1). Patients who attained remission on day 28 had 55% survival at the end of 48 months compared to those who had persistent disease on day 28 (16% survival). Analysis of risk stratification of patients showed that those in favorable risk, intermediate risk and adverse risk had overall survival of 80%, 39% and 21% respectively at the end of 48 months.
Conclusions
Day 5 peripheral blood blasts and day 14 bone marrow status are most important factors that help predicting remission on day 28 in patients with AML, surpassing the prognostic information obtained from analysis of pretreatment characteristics alone. Day 14 bone marrow blasts can be used as a surrogate marker in predicting overall survival and disease free survival. Also, day 14 bone marrow studies can help in identifying subset of patients who can be benefit from HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal